Image Source: drjockers.com
Can Exercise Help Gastroparesis? Find Out
Yes, exercise can help with gastroparesis by improving stomach emptying, boosting intestinal motility, and aiding in overall digestive health. However, it’s crucial to approach physical activity with caution and in consultation with your doctor.
Grasping Gastroparesis and the Role of Movement
Gastroparesis, a chronic gastrointestinal motility disorder, affects how your stomach empties food. Normally, strong muscle contractions move food through your digestive tract. In gastroparesis, these contractions are weakened, leading to delayed stomach emptying. This can cause a range of uncomfortable symptoms, including bloating, early fullness, nausea, vomiting, abdominal pain, and even fluctuations in blood sugar levels, particularly in individuals with diabetes.
The idea of exercising with a condition that already causes digestive distress might seem counterintuitive. Many people with gastroparesis struggle with low energy, fatigue, and the very symptoms that exercise aims to alleviate. However, emerging research and anecdotal evidence suggest that a tailored approach to physical activity can offer significant benefits. The key lies in understanding what types of exercise are appropriate and how to gradually introduce them into your routine.
The Science Behind Movement and Stomach Emptying
How exactly does physical activity influence stomach emptying and overall digestive health? The connection is multifaceted.
Enhancing Intestinal Motility
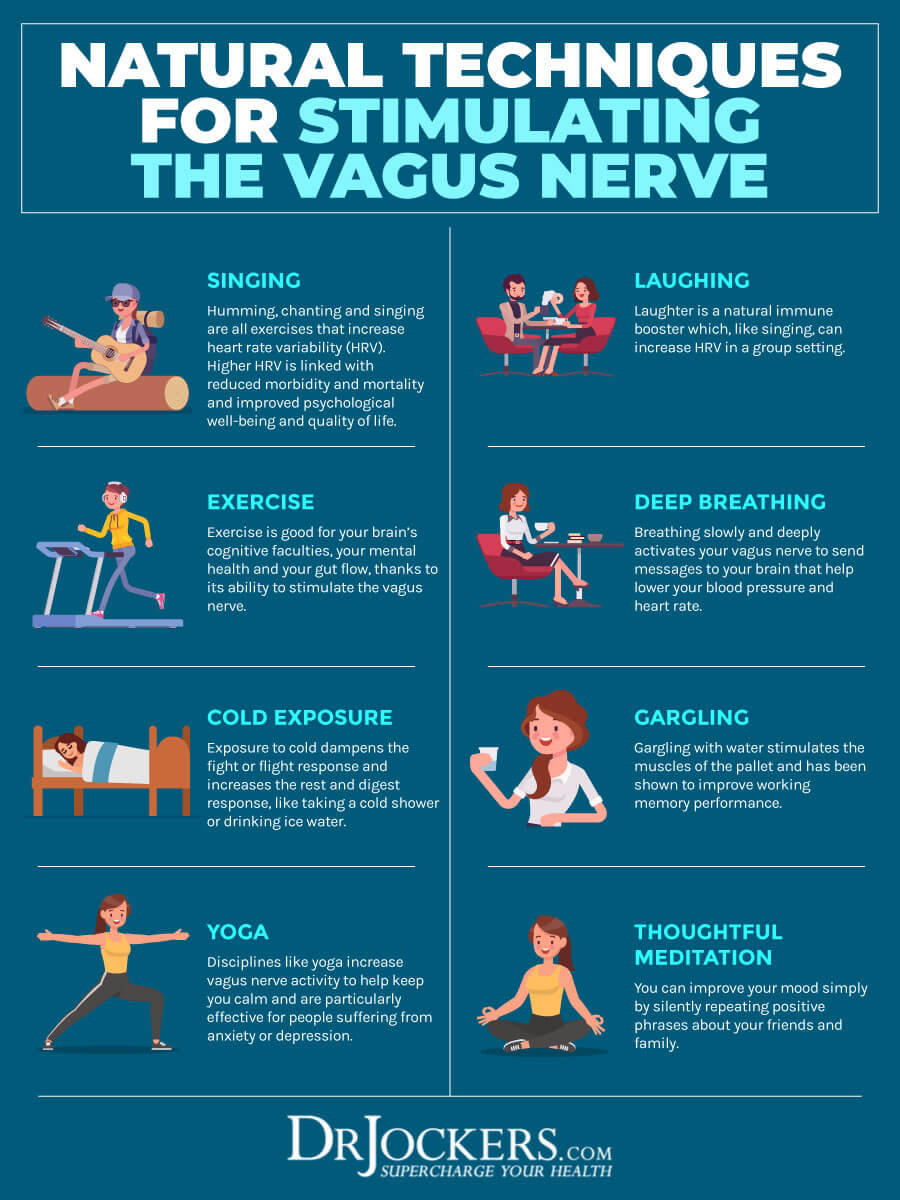
Your gastrointestinal tract relies on a complex series of muscular contractions to propel food and waste along. This process is known as intestinal motility. When motility is impaired, as in gastroparesis, digestion slows down. Exercise, particularly aerobic activity, can stimulate the vagus nerve, a key player in regulating digestion. By activating the vagus nerve, exercise can potentially increase the frequency and strength of these muscular contractions, thereby improving stomach emptying.
Improving Blood Flow to Digestive Organs
Exercise increases blood circulation throughout the body. This improved blood flow can also benefit the stomach and intestines, providing them with more oxygen and nutrients. Enhanced blood supply can support the function of the digestive muscles and aid in the overall efficiency of the digestive system.
Stress Reduction and its Digestive Impact
Chronic stress is a known contributor to gastrointestinal motility disorders. It can disrupt the gut-brain axis, affecting nerve signals and muscle function in the digestive tract. Many forms of exercise are excellent stress relievers. By reducing stress levels, exercise can indirectly improve digestive health and potentially alleviate some gastroparesis symptoms.
Blood Sugar Regulation in Diabetic Gastroparesis
For individuals whose gastroparesis is linked to diabetes, exercise plays a vital role in blood sugar control. Better blood sugar management can, in turn, help stabilize and potentially improve nerve function in the digestive system, which is often damaged by prolonged high blood sugar.
Types of Exercise to Consider for Gastroparesis
Not all exercises are created equal when it comes to managing gastroparesis. The focus should be on low-impact, gentle activities that won’t exacerbate symptoms.
Gentle Aerobic Activities
- Walking: This is often the most accessible and beneficial form of exercise. Start with short, slow walks and gradually increase the duration and pace as your body tolerates it. Aim for consistency rather than intensity.
- Swimming: The buoyancy of water can be very supportive, reducing stress on joints and making movement feel easier. It’s an excellent cardiovascular workout that can also help with nausea relief due to its calming effect.
- Cycling (Stationary or Gentle Outdoor): A stationary bike is a good option for controlled exercise. If cycling outdoors, choose flat, low-traffic routes.
- Water Aerobics: Combines the benefits of swimming with guided movements, often in a group setting which can provide motivation.
Strength Training (Light and Focused)
While intense weightlifting might not be suitable, light strength training can be beneficial for overall health and posture, which can indirectly support digestion. Focus on:
- Bodyweight exercises: Squats, lunges (modified if needed), push-ups against a wall.
- Resistance bands: Offer a versatile way to build strength without heavy weights.
- Light dumbbells: Focus on controlled movements and proper form.
It’s crucial to avoid exercises that involve jarring movements or significant abdominal pressure, especially immediately after eating.
Mind-Body Practices
These practices are excellent for stress reduction and improving body awareness, which can be very helpful for managing chronic conditions.
- Yoga: Focus on gentle, restorative poses. Avoid inversions or poses that put pressure on the abdomen if they trigger symptoms. Certain poses can aid in gentle massage of the abdominal organs.
- Tai Chi: A slow, flowing martial art that emphasizes balance, coordination, and deep breathing. It promotes relaxation and can improve intestinal motility through its gentle movements.
- Pilates: Focuses on core strength and controlled movements. Modified Pilates routines can be very beneficial.
When to Exercise and What to Avoid
Timing and type of exercise are critical for individuals with gastroparesis.
Recommended Timing
- Avoid exercising immediately after meals: This is paramount. Give your stomach adequate time to begin emptying. A window of 1-2 hours after a small, easily digestible meal is often recommended.
- Listen to your body: If you feel nauseous or uncomfortable, it’s not the right time to exercise.
- Consider exercising on an empty stomach: Some individuals find that exercising before their first meal of the day is well-tolerated. However, this depends on your energy levels and usual dietary pattern.
Exercises to Approach with Caution or Avoid
- High-impact activities: Running, jumping, and intense aerobics can jostle the stomach and potentially worsen symptoms like nausea and vomiting.
- Exercises that involve significant bending or inversions: These can increase intra-abdominal pressure and may lead to reflux or discomfort.
- Heavy weightlifting: The straining involved can increase pressure on the abdomen and may not be suitable.
- Intense or prolonged exercise: Overexertion can lead to fatigue and exacerbate symptoms.
Creating a Safe and Effective Exercise Plan
Developing a personalized exercise plan requires careful consideration of your individual condition and medical advice.
Consultation with Healthcare Professionals
- Doctor: Your primary physician or gastroenterologist is your first point of contact. They can assess your gastroparesis severity, identify any underlying causes, and advise on the suitability of exercise.
- Registered Dietitian: A dietitian can help you adjust your dietary changes to complement your exercise routine, ensuring you have adequate energy without overloading your digestive system. They can also advise on optimal timing for meals relative to exercise.
- Physical Therapist: A PT specializing in pelvic floor or gastrointestinal issues can provide tailored exercise recommendations and demonstrate proper form.
Gradual Progression
- Start slow and low: Begin with short durations (e.g., 5-10 minutes) and low intensity.
- Increase gradually: As your body adapts, slowly increase the length of your sessions and then the intensity.
- Consistency over intensity: Aim for regular, moderate physical activity rather than occasional, strenuous workouts.
Hydration and Nutrition
- Stay hydrated: Drink plenty of water before, during, and after exercise, especially if you experience vomiting.
- Fuel appropriately: Ensure your dietary changes support your energy needs for exercise. Small, frequent meals that are easy to digest are often recommended.
Monitoring Symptoms
- Keep a symptom diary: Track your exercise sessions alongside your gastroparesis symptoms (nausea, pain, bloating, stomach emptying time). This helps identify which activities and timings are beneficial or detrimental.
- Be mindful of post-exercise symptoms: Pay attention to how you feel in the hours after exercising.
Exercise Benefits Beyond Stomach Emptying
The positive effects of exercise extend far beyond direct impacts on stomach emptying.
- Improved Mood and Mental Well-being: Chronic illness can take a toll on mental health. Exercise is a powerful mood booster, releasing endorphins that combat anxiety and depression.
- Enhanced Sleep Quality: Regular physical activity can help regulate sleep patterns, leading to more restful sleep, which is crucial for healing and overall well-being.
- Weight Management: For some with gastroparesis, weight loss is a concern due to poor nutrient absorption. Controlled exercise can help maintain a healthy weight and build muscle mass.
- Increased Energy Levels: While it may seem counterintuitive, regular exercise can combat fatigue and improve overall stamina.
- Better Blood Sugar Control: As mentioned, this is a critical factor for diabetic gastroparesis, but stable blood sugar benefits everyone.
- Bladder Training (Indirect Benefit): While not directly linked to gastroparesis, improved core strength from exercises like Pilates can indirectly support pelvic floor health. Strengthening these muscles can also contribute to better overall body control and potentially alleviate some secondary discomforts. This is sometimes referred to as bladder training in a broader sense of improving pelvic floor function.
Case Studies and Research Insights
While extensive large-scale clinical trials specifically on exercise and gastroparesis are still developing, smaller studies and expert consensus point towards its benefits.
- Diabetic Gastroparesis Studies: Research focusing on diabetic gastroparesis has shown that consistent exercise improves glycemic control, which is a major factor in managing this condition. Some studies suggest that improved glycemic control itself can positively impact intestinal motility.
- Gastrointestinal Motility Disorders and Vagal Tone: Studies on the vagus nerve indicate that aerobic exercise can enhance vagal tone, the activity of the vagus nerve. A healthy vagal tone is essential for proper digestive health, including regulating stomach emptying.
- Qualitative Data: Patient testimonials and surveys often highlight that individuals who successfully incorporate gentle exercise into their lives report better symptom management, including significant nausea relief and improved quality of life.
Adapting Exercise for Specific Gastroparesis Symptoms
Here’s how you might adapt exercise based on specific symptoms:
| Symptom | Exercise Modifications | Recommended Activities |
|---|---|---|
| Nausea/Vomiting | Avoid exercise immediately after eating. Focus on very gentle, slow movements. Stay hydrated. Consider sitting or lying down exercises if standing is too much. | Gentle walking, seated chair exercises, Tai Chi. |
| Bloating/Fullness | Avoid exercises that increase intra-abdominal pressure. Focus on movements that encourage gentle digestion. | Gentle stretching, walking, restorative yoga. |
| Abdominal Pain | Listen to your body intently. Stop if any movement exacerbates pain. Focus on deep breathing and relaxation techniques. | Light stretching, deep breathing exercises, gentle walking. |
| Fatigue/Low Energy | Start with very short sessions (5-10 minutes). Break up activity into smaller chunks throughout the day. Prioritize rest. | Chair exercises, very short, slow walks, mindful movement. |
| Dizziness/Lightheadedness | Ensure adequate hydration and electrolyte balance. Avoid sudden changes in position. Have a chair or support nearby. | Seated exercises, slow movements, mindful breathing. |
Integrating Exercise with Dietary Changes
Dietary changes are a cornerstone of gastroparesis management. Exercise should complement, not contradict, these changes.
- Timing of Meals and Exercise: As stressed before, avoid eating large meals immediately before exercise. Smaller, nutrient-dense meals or snacks several hours before can provide energy.
- Food Choices: Stick to the recommended gastroparetic diet (often low-fat, low-fiber, easily digestible foods) even on exercise days. Your dietitian can help you plan meals around your activity.
- Hydration: Essential for everyone, but especially important with gastroparesis and exercise. Dehydration can worsen digestive symptoms.
Challenges and Overcoming Them
It’s important to acknowledge the hurdles individuals with gastroparesis may face when trying to exercise.
- Lack of Energy and Fatigue: This is a common complaint. Starting small and celebrating minor victories is key.
- Fear of Symptom Exacerbation: This is a valid concern. A slow, gradual approach with close monitoring is essential.
- Motivation: When you don’t feel well, finding the motivation to move can be incredibly difficult. Having a support system, exercising with a friend, or joining a gentle group class can help.
- Gastrointestinal Upset: If exercise consistently triggers symptoms, reassess the type, intensity, and timing with your healthcare provider.
A Personalized Path to Movement
Ultimately, the question of “Can exercise help gastroparesis?” has a positive answer, but with important caveats. It’s not a one-size-fits-all solution.
- Consult Your Doctor: This is the absolute first step.
- Work with a Dietitian: Optimize your nutrition to support your body.
- Start Gently: Begin with minimal duration and intensity.
- Listen to Your Body: Never push through significant pain or nausea.
- Be Consistent: Regular, gentle movement is more beneficial than sporadic, intense bursts.
- Track Your Progress: Use a diary to monitor symptoms and identify what works.
- Celebrate Small Wins: Every bit of progress counts.
By carefully integrating appropriate physical activity into a comprehensive management plan that includes tailored dietary changes, individuals with gastroparesis can potentially improve their stomach emptying, enhance their intestinal motility, and significantly improve their overall digestive health and quality of life. The journey may require patience and adjustments, but the exercise benefits can be substantial.
Frequently Asked Questions (FAQ)
Q1: Is it safe to exercise with gastroparesis?
A1: Yes, it can be safe and beneficial to exercise with gastroparesis, but only with your doctor’s approval and under their guidance. The type, intensity, and timing of exercise are crucial.
Q2: What are the best types of exercise for gastroparesis?
A2: Gentle, low-impact activities like walking, swimming, stationary cycling, gentle yoga, and Tai Chi are often recommended. Focus on consistency rather than intensity.
Q3: When should I exercise if I have gastroparesis?
A3: It’s generally best to avoid exercising immediately after eating. Wait at least 1-2 hours after a small meal, and listen to your body. Some people prefer exercising on an empty stomach.
Q4: Can exercise help reduce nausea from gastroparesis?
A4: Yes, for some individuals, gentle exercise can help reduce nausea by improving intestinal motility, reducing stress, and promoting overall well-being. However, strenuous exercise can worsen nausea for others.
Q5: How much exercise should I do?
A5: Start with very short durations (5-10 minutes) and low intensity. Gradually increase as your body tolerates it. Consistency is more important than duration or intensity.
Q6: What should I do if exercise makes my symptoms worse?
A6: If exercise exacerbates your symptoms, stop the activity and consult your doctor or a physical therapist. You may need to adjust the type, intensity, or timing of your exercise.
Q7: Does exercise affect blood sugar levels in gastroparesis patients?
A7: Yes, especially for those with diabetic gastroparesis. Exercise can help improve blood sugar control, which is important for nerve health and can indirectly benefit digestive health.
Q8: Can exercise help with slow stomach emptying?
A8: Emerging research suggests that exercise can positively influence intestinal motility and potentially improve stomach emptying by stimulating the vagus nerve and increasing blood flow to the digestive organs.
Q9: Should I make dietary changes alongside starting an exercise program?
A9: Yes, it’s highly recommended to work with a registered dietitian to ensure your dietary changes support your exercise routine and overall gastroparesis management.
Q10: How does exercise improve overall digestive health in gastroparesis?
A10: Exercise can improve digestive health by enhancing intestinal motility, reducing stress, improving blood circulation to the gut, and promoting a healthier gut-brain axis, contributing to better symptom management.